This guide aims to cut through the confusion by offering an in-depth look at what coronavirus is and what makes COVID-19 unique.
You’ll learn how this disease spreads and what symptoms to watch out for. Along with how to prepare with proper prevention and response strategies.
You’ll also learn how to apply the hierarchy of control to help you further mitigate the risks associated with COVID-19.
What is COVID-19?
In late 2019, a new virus (since named COVID-19) emerged. By early 2020, it was making headlines across the globe.
But this isn’t the first time a coronavirus has sparked worldwide alarm. So, let’s start from the beginning by unpacking what a coronavirus is.
What are Coronaviruses?
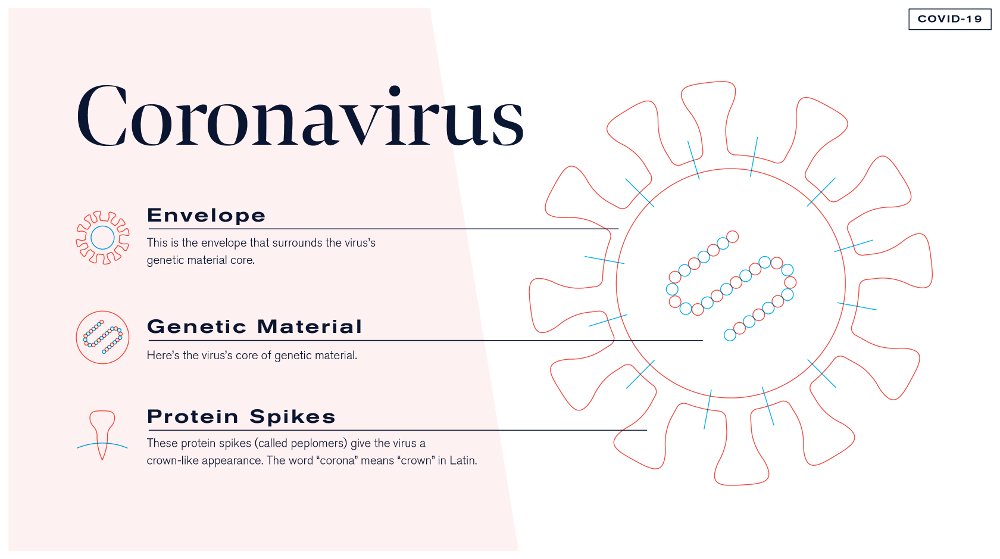
A coronavirus is part of a large group of viruses that are zoonotic, which means that they’re transmitted between animals and people.
Rarely, a coronavirus jumps from animals to people – and that’s called a spillover event. Spillover events happen because of a mutation in the virus or increased contact between the infected animals and humans. Once a coronavirus develops in people, it then starts spreading from person to person.
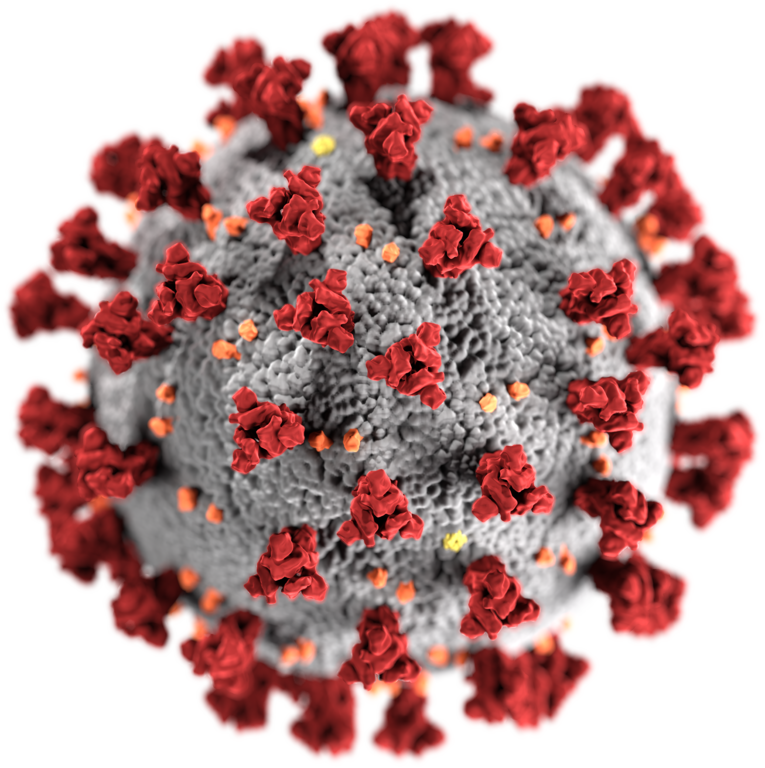
Where does the Coronavirus gets its name from?
The coronavirus gets its name from its appearance…
Coronavirus examples
According to the World Health Organization (WHO), coronaviruses tend to be mild and cause minor respiratory and gastrointestinal diseases. However, there are some types of viruses that are more severe and dangerous, such as SARS and MERS.
SARS-CoV
MERS-CoV
COVID-19
Adding to the list of known coronaviruses (of which there are seven), a new virus was identified in 2019.
This new virus is named SARS-CoV-2, and it’s not yet pinned to a specific animal source. The associated disease is called “coronavirus disease 2019,” which is abbreviated as COVID-19:
- “CO” stands for “corona”
- “VI” stands for “virus”
- “19” stands for 2019
- “D” stands for “disease”
How COVID-19 spreads
COVID-19 is a new disease, so researchers are still learning how it spreads. So far, it’s believed that the virus mainly spreads from person-to-person. And less commonly, via contaminated objects and surfaces. Current understanding is based on early case reports and knowledge of how similar coronaviruses spread.
What we know, and don't know
Contact with contaminated objects and surfaces
The virus is able to spread through contaminated objects and surfaces. This could happen if an uninfected person came in contact with the virus on a phone, table, door handle, or another surface – and then touched their mouth, nose, or eyes. However, this mode of transmission is less common than person-to-person transmission.
Studies suggest that the COVID-19 virus may persist on surfaces for a few hours or up to several days. This may vary under different conditions (e.g. type of surface, temperature or humidity of the environment).

How contagious is COVID-19?
Health officials and scientists measure the spread of a disease using R0—pronounced “R naught.” This is a statistical estimate of how quickly a disease spreads if left unchecked. If R0 is less than 1, then the spread of the disease typically will die out. But if R0 is greater than 1, then each sick person, on average, will infect at least one other person (who then infects others).
Prevention
Taking precautions to protect yourself from COVID-19 isn’t alarmist – it’s responsible.
Practice healthy habits
The hierarchy of control and COVID-19
#1 - Elimination
During the COVID-19 pandemic, ‘Elimination’ as a control measure is not feasible for the workplace. It simply doesn’t seem practicable for an individual business to completely eliminate a virus.
#2 - Substitution

Again. during the COVID-19 pandemic, ‘Substitution’ as a control measure is not feasible for the workplace. It simply doesn’t seem practicable for an individual business to substitute a virus for something better. However, substitution does play apart for consumers. With the rapidly growing availability of home deliveries, consumers certainly don’t have to go without necessities or even luxuries whilst self isolating.
Although it may seem impracticable at first glance, operational strategies focused around substitution of COVID-19 hazards are popping up. And they’re even starting to changing the way we not only shop but also how businesses operate and keep their staff safe.
#3 - Engineering controls

This has become a highly regarded control measure to protect against COVID-19.
In almost every store and small shop there’s been physical shields and barriers installed. Most commonly in the form of clear plastic guards and covers, protecting staff from customers (and visa-versa).
Engineering technologies have also had a part to play in providing engineering control measures. Most notably in the form of contactless card payments – removing the need to handle cash.
But there’s also a growing demand for on site ordering apps and home delivery systems. Such systems will become ever more prevalent as the hospitality industry begins to open up again and rethinks how it interacts with its consumers.
#4 - Administration

Administrative control measures have been pivotal in turning the tide and reducing the spread of infections. The most significant of which has been social distancing.
Social distancing has been an administrative control, implemented by the government, aimed at changing how we all interact in order to reduce the risk of COVID-19 spreading.
In fact a whole host of administrative controls have been put in place across a wide range of industries. These include…
- 2m/6.5ft gap floor markings
- Increase in restricted access zones
- Elderly, vulnerable & NHS shopping hours
- Hand washing & sanitizer stations
- One-way pedestrian systems
- Re-organisation of layouts
- Limited browsing hours
- Signage
#5 - PPE, the last resort

As with any strategy to control hazards within the workplace, PPE is the last resort.
As touched on in the previous lesson, PPE is often ineffective. If controls can be implemented in other areas of the hierarchy, there should be no need for PPE.
Utilising PPE as a primary control strategy can have the undesired effect of giving employees and the public a false sense of security. The consequences of which can lead to increase risk of infection and an increased chance of passing on COVID-19.
On the whole, everybody is acting with caution – washing hands more regularly, maintaining social distancing and paying by card.
Adding PPE and providing a false sense of security can undermine this collaborative effort. And, as discussed in the previous lesson, improper use of PPE can increase risks those who are trying to avoid them.
Our advice is be cautious when opting for PPE as a control measure. Always ask yourself this…
“Can I further use the hierarchy of control to mitigate the risks and reduce the requirement for PPE”
Information for businesses
Companies have a responsibility to their employees to keep them safe, especially during a health crisis. As a result, COVID-19 is leading many businesses to rethink their employees’ health and safety at work.
In general, there’s a low risk of contracting COVID-19 at work, but because employees are often in close quarters (sharing offices, collaborating in meetings, and more) businesses could contribute to the disease’s spread.
Workers who are most at risk
Professions with a higher risk of spreading COVID-19 include:
- Health care (examples: clinical laboratory personnel, medical transport workers, health care providers, support staff)
- Death care (examples: coroners, medical examiners, funeral directors)
- Airline operations
- Waste management
Getting the workplace ready
How to respond if an employee gets sick
If someone becomes unwell in the workplace with a new, continuous cough or a high temperature, they should be sent home and advised to follow the advice to stay at home.
Consider alternate working arrangements
Create a contingency plan
How will you keep your business running if COVID-19 impacts your area?
Employees, contractors, and suppliers may not be able to come to your place of business due to local restrictions or because they’re ill. Explore possible worst-case scenarios and the steps you would take in each situation to maintain operations. When your plan is complete, be sure to share it with your employees and other stakeholders.
Actively encourage sick employees to stay home
The Public Health England recommends that employers:
- Encourage employees to stay home if they have a temperature above 37.5’C or respiratory symptoms, such as coughing, sneezing, or shortness of breath.
- Send employees home if they develop cold or flu-like symptoms at work. You can check your employees’ temperature using a hand-held thermal scanner.
- Keep in mind that a combination of symptoms (elevated temperature and respiratory issues) is the best indicator of infection.